Introduction
Embark on a thorough exploration of the multifaceted world of ringworm and fungal infections. This in-depth guide is designed to provide a comprehensive understanding of the causes, symptoms, and treatment options for these prevalent yet often underestimated health conditions. By delving into the complexities, we aim to empower individuals to make informed decisions about their well-being.
Ringworm and Tinea Fungal Infections
Dive into the nuanced landscape of fungal infections, including ringworm, athlete’s foot, and fungal nail infections. Each condition unfolds a unique narrative, demanding tailored approaches for effective management.
Causes and Spread
- Direct Skin Contact: Fungal spores exploit direct skin contact, necessitating vigilant personal hygiene practices.
- Shared Objects: Everyday items like towels and combs become potential carriers, emphasizing the need to avoid shared personal belongings.
- Pets as Vectors: Household pets, such as dogs and cats, can harbor ringworm, acting as vectors for transmission.
- Environmental Influences: Fungal spores thrive in warm and moist environments, elucidating their prevalence in communal spaces like gym changing rooms.
Who is at Risk?
- Age Considerations: While children are more susceptible, fungal infections do not discriminate and can affect individuals of all age groups.
- Ethnic Disparities: Certain infections, like scalp infections (tinea capitis), exhibit a higher prevalence among African-Caribbean children.
- Gender Dynamics: Groin infections tend to be more common in young men.
- Health Conditions: Individuals with weakened immune systems, such as those with HIV or AIDS, face elevated susceptibility.
Recognizing Symptoms
- Ringworm on the Skin: Manifests as round, red, or silvery patches accompanied by itching and inflammation.
- Fungal Scalp Infections: Characterized by scaly patches, patchy hair loss, and persistent itchiness.
- Athlete’s Foot: Presents as an itchy, dry, red rash, with potential blisters and scaling.
- Jock Itch: Recognizable through red-brown sores and itchiness around the groin area.
- Fungal Nail Infections: Indicators include thickened, discolored nails with potential brittleness.

When to Consult a Doctor
- Fungal Scalp Infections: Immediate consultation is imperative, as these often require prescription antifungal tablets.
- Persistent Infections: If symptoms persist after two weeks of over-the-counter treatment, seeking medical advice is crucial.
- Immunocompromised Individuals: Those with conditions like HIV, AIDS, or undergoing immune-weakening treatments should seek prompt medical attention.
Treatment Options
- Ringworm on the Skin: Over-the-counter antifungal creams prove effective for mild cases.
- Athlete’s Foot and Groin Infections: Antifungal creams, gels, or sprays recommended for two weeks, with the possibility of additional antifungal tablets if symptoms persist.
- Fungal Scalp Infections: Treatment involves antifungal tablets and specialized shampoos, each tailored to the specific fungi.
- Fungal Nail Infections: Combining antifungal nail paint and tablets often proves effective for severe cases.
Comparative Table – Treatment Options
| Type of Infection | Treatment Method | Duration | Possible Side Effects |
|---|---|---|---|
| Ringworm | Antifungal Cream | 2 weeks | Mild irritation |
| Athlete’s Foot | Antifungal Spray | 2 weeks | Dryness, itching |
| Fungal Nail | Antifungal Tablets | Varies | Headache, nausea |
| Scalp Infection | Antifungal Shampoo | 2 weeks | Prevention and recovery |
Preventing Spread
- Personal Hygiene Practices: Regularly wash and thoroughly dry affected areas, adhering to stringent personal hygiene practices.
- Avoiding Shared Items: Refrain from sharing personal items like combs, towels, and clothing to mitigate the risk of transmission.
- Pet Care Awareness: Promptly attend to pets exhibiting ringworm symptoms, minimizing the risk of human transmission.
- Environmental Hygiene: Maintain good hygiene in shared spaces like gym and swimming pool changing rooms to curb the spread of infections.

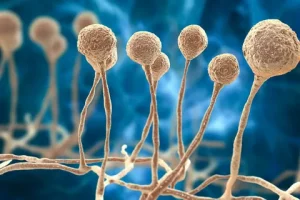
Diagnosing and Understanding
- Diagnostic Process: Uncover the process by which medical professionals diagnose fungal infections, including microscopic analysis.
- Risk Groups: Identify factors contributing to heightened vulnerability, encompassing age, existing health conditions, and past fungal infections.
- Spread Mechanisms: Unravel the intricate ways fungi spread, guiding preventive strategies and informed decision-making.
Conclusion
In conclusion, this extensive guide equips readers with a profound understanding to combat and prevent ringworm and fungal infections. By fostering awareness and promoting informed decision-making, individuals can actively manage their health, paving the way for a happier and healthier life.




