Introduction:
Tularemia, colloquially known as rabbit fever or deer fly fever, is a relatively rare infectious disease brought about by the bacterium Francisella tularensis. This comprehensive guide aims to unravel the complexities of tularemia, shedding light on its causes, symptoms, and effective preventive measures.
Causes:
Understanding the origins of tularemia is crucial to its prevention. While humans can indeed contract the disease, it is not a natural occurrence in our species. The primary carriers of the bacterium are animals, including rabbits, rodents, sheep, and birds. Even common house pets like dogs and cats are susceptible to tularemia.
The ways in which individuals can become infected with tularemia are diverse:
- Insect Bites: Particularly from deer flies or ticks.
- Contact with Infected Animals: Handling the skin, hair, or meat of an infected animal can transmit the bacteria.
- Consuming Contaminated Water or Food: Undercooked meat or contaminated water sources pose risks of infection.
- Inhalation of Bacteria: During activities such as construction or gardening, bacteria from the soil can become airborne.
- Laboratory Exposure: Individuals working in laboratory settings may face risks of infection.
- Potential Bioterrorism Acts: In rare instances, intentional exposure to the bacteria may occur.

To gain a holistic understanding, the following comparative table outlines the various transmission methods:
Comparative Table: Causes of Tularemia
| Transmission Method | Common Vectors |
|---|---|
| Insect Bites | Deer flies, ticks |
| Contact with Animals | Infected animal skin/meat |
| Contaminated Water/Food | Undercooked meat, water |
| Inhalation | Soil during construction |
| Laboratory Exposure | Research settings |
Geographical Impact:
Tularemia is not confined to specific regions; it can occur anywhere in the world. However, it is most prevalent in rural areas where animals are more likely to carry the bacterium. The resilience of Francisella tularensis in soil, water, and deceased animals for weeks contributes to the varied pathways through which infections can occur.
Symptoms:
The manifestation of tularemia symptoms is influenced by the method of infection. It is important to note that exposure to the bacteria does not guarantee the onset of the disease. If symptoms do occur, they typically surface within 3 to 5 days but can take up to 2 weeks. There are several types of tularemia, each with its distinct set of symptoms:
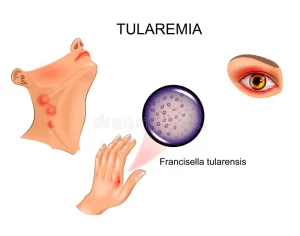
- Ulceroglandular Tularemia (Most Common):
- Skin ulcers, often caused by bites from infected animals or insects.
- Painful and swollen lymph glands.
- Fever, chills, headache, and fatigue.
- Oculoglandular Tularemia:
- Eye-related symptoms, including pain, swelling, discharge, and redness.
- Formation of ulcers inside the eyelid.
- Tender lymph glands around the ear, neck, and jaw.
- Oropharyngeal Tularemia:
- Affects the mouth, throat, and digestive system.
- Symptoms may include throat pain, vomiting, diarrhea, swollen tonsils or lymph nodes in the neck, and ulcers in the mouth.
- Often caused by consuming undercooked meat from a wild animal or drinking contaminated water.
- Pneumonic Tularemia:
- Symptoms similar to pneumonia, including trouble breathing, chest pain, and a dry cough.
- Typhoidal Tularemia (Rare and Serious):
- Symptoms may include an enlarged spleen or liver, diarrhea, vomiting, severe fatigue, and elevated fever.
Comparative Table: Types of Tularemia and Their Symptoms
| Type | Symptoms |
|---|---|
| Ulceroglandular | Skin ulcers, swollen lymph glands, fever |
| Oculoglandular | Eye pain, swelling, redness, lymph node tenderness |
| Oropharyngeal | Throat pain, vomiting, diarrhea, swollen tonsils |
| Pneumonic | Difficulty breathing, chest pain, dry cough |
| Typhoidal | Enlarged spleen/liver, diarrhea, severe fatigue |
Who’s at Risk?:
Although tularemia is rare, certain factors increase the risk of exposure. In the United States, approximately 200 cases are reported annually, with the primary transmission modes being tick bites or contact with contaminated animals. Individuals at higher risk include:
- Occupations: Laboratory workers, farmers, veterinarians, hunters, landscapers, wildlife managers, and meat handlers.
- Geographical Location: Residents or visitors in the south-central United States.
- Activities: Hunting or gardening, as wild animals may carry tularemia, and soil disturbance may release bacteria.

Diagnosis and Treatment:
Diagnosing tularemia can be challenging due to symptom similarities with other diseases. Doctors typically conduct tests to confirm the presence of the bacteria, and chest X-rays may be ordered to check for signs of pneumonia.
Treatment primarily involves antibiotics, administered either by injection or orally. In cases where complications such as pneumonia or meningitis arise, specific treatments for these conditions are necessary. Interestingly, individuals who have had tularemia often develop immunity, Treatment for other medical problems although rare instances of recurrence may occur.

Prevention:
Mitigating the risk of tularemia involves adopting proactive measures:
- Safe Handling: Avoid using bare hands to skin or dress wild animals.
- Animal Interaction: Steer clear of sick or dead animals.
- Protective Clothing: Wear clothing that covers exposed skin, with special attention to tight fits at the wrists and ankles.
- Insect Repellents: Utilize insect repellents to minimize the risk of insect bites.
- Tick Management: Promptly remove ticks.
- Hygiene Practices: Ensure the consumption of clean water and fully cooked wild meats.
Conclusion:
In conclusion, comprehending tularemia is essential for its prevention and early intervention. By unraveling its causes, diverse symptoms, and implementing proactive preventive measures, individuals can safeguard themselves against this rare infectious disease. Awareness and education play pivotal roles in minimizing the impact of tularemia on public health.