Introduction:
Brucellosis, an infectious disease caused by the Brucella bacteria, remains a relatively rare yet significant health concern. Primarily transmitted from animals to humans, understanding its various facets is crucial for early detection, effective treatment, and prevention. This comprehensive guide explores the causes, symptoms, treatment options, and preventive measures associated with brucellosis.
Causes of Brucellosis:
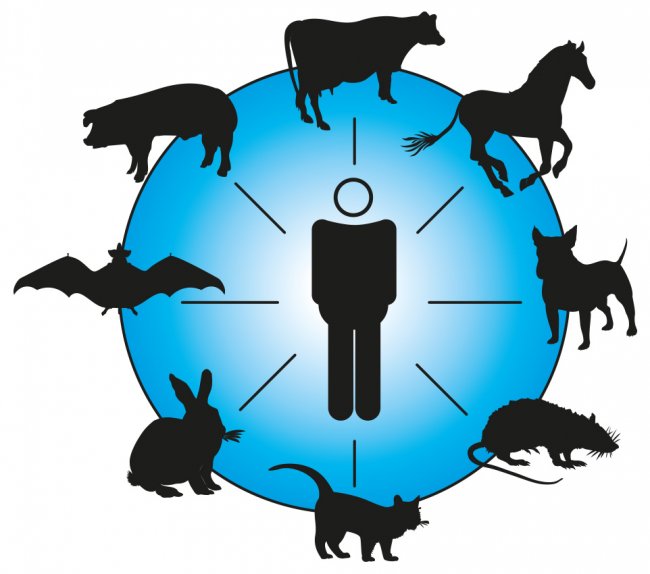
Brucellosis is triggered when individuals come into contact with animals or their products infected with the Brucella bacteria. The bacteria can infiltrate the body through various means, such as cuts or scratches in the skin, inhalation of contaminated air (though rare), or consumption of unpasteurized products like milk or undercooked meat. The disease is associated with different strains of Brucella bacteria, each commonly found in specific animal hosts and geographical regions.

Types of Brucella Bacteria:
Understanding the diverse strains of Brucella is essential to comprehend the varied manifestations of the disease. The primary culprits include:
- B. melitensis: This strain, prevalent in sheep and goats, is responsible for the majority of human brucellosis cases. It is often found in regions like Spain, Greece, Latin America, the Middle East, and India.
- B. suis: Commonly found in wild pigs, this strain is the most frequently reported in the United States, particularly in the Southeast and California. It also occurs in Europe, South America, and Southeast Asia.
- B. canis: Associated with dogs, this strain is observed in North, Central, and South America, Japan, and Central Europe.
- B. abortus: Originating from cattle, this strain is widespread globally but has been eradicated in several countries, including parts of Europe, Japan, Israel, Canada, Australia, and New Zealand.
Risk Factors:
Several factors increase the likelihood of contracting brucellosis:
- Consumption of unpasteurized dairy products from infected animals.
- Consumption of unpasteurized cheeses, especially those from high-risk regions like the Mediterranean.
- Traveling to areas where Brucella is common.
- Working in meat-processing plants or slaughterhouses.
- Employment on a farm.
Brucellosis has also been reported in specific occupational groups, such as hunters in the U.S. and veterinarians who have immunized cattle with the Brucella vaccine.
Can I Get Brucellosis From My Dog?:
While dogs can indeed be infected with B. canis, the transmission of brucellosis from dogs to humans is uncommon. Pet owners should exercise caution, particularly those with weakened immune systems. Veterinarians, due to their close contact with animals, face an increased risk of contracting the disease.
Symptoms of Brucellosis:
Recognizing the symptoms of brucellosis is crucial for early detection and treatment. Symptoms may vary in severity, and the onset usually occurs within five to 30 days after exposure to the bacteria. The key symptoms include:
- Fever: The most common symptom, often characterized by high spikes that typically occur in the afternoon.
- Back pain: A prevalent symptom associated with brucellosis.
- Body-wide aches and pains: Muscular discomfort and pain throughout the body.
- Poor appetite and weight loss: Loss of appetite leading to a noticeable decrease in weight.
- Headache: Persistent headaches may be indicative of brucellosis.
- Night sweats: Excessive sweating during the night, often accompanied by fever.
- Weakness: A general feeling of fatigue and weakness.
- Abdominal pain: Discomfort and pain in the abdominal region.
- Cough: In some cases, a persistent cough may be present.
The severity of symptoms depends on the specific type of Brucella causing the infection. For instance, B. abortus typically causes mild or moderate symptoms, which may become chronic. On the other hand, B. melitensis may result in sudden and severe symptoms, potentially leading to disability.

Diagnosis and Treatment:
Diagnosing brucellosis involves a thorough examination by a healthcare professional. Physical assessments may reveal swollen liver, lymph nodes, and spleen, along with unexplained fever, joint swelling and pain, and rash. Blood tests are crucial to confirm the infection and identify the specific strain of Brucella.
Treatment of brucellosis can be challenging, requiring a prolonged course of antibiotics. Commonly used antibiotics include doxycycline, streptomycin, ciprofloxacin, rifampin, sulfamethoxazole/trimethoprim, and tetracycline. A combination of doxycycline and rifampin is often prescribed for 6-8 weeks. Completing the entire course of antibiotics is crucial to prevent relapse, with the rate of relapse after treatment ranging from 5-15%.
Recovery from brucellosis can take weeks or even months. Timely initiation of treatment, preferably within one month of symptom onset, increases the chances of a complete cure.

Complications of Brucellosis:
Severe cases of brucellosis may lead to complications such as infections of the central nervous system, endocarditis (infection of the heart lining or valves), and liver abscesses. Furthermore, brucellosis can result in long-lasting symptoms resembling systemic exertion intolerance disease (formerly known as Myalgic Encephalomyelitis/Chronic Fatigue Syndrome), potentially leading to disability. Pregnant women with brucellosis face the risk of miscarriage or birth defects in the baby.
While death from brucellosis is uncommon, fatalities are typically associated with endocarditis.
Prevention:
Preventing brucellosis involves adopting several precautionary measures:
- Avoiding unpasteurized products: Refrain from consuming unpasteurized dairy products or cheeses, especially those originating from high-risk regions.
- Protective gear in the workplace: Individuals working in the animal processing industry should wear rubber gloves to minimize the risk of exposure.
- Seeking medical attention: If individuals come into contact with an animal infected with Brucella, it is imperative to inform healthcare providers, even in the absence of symptoms. Monitoring for at least six months may be recommended.
Unfortunately, there is no effective human vaccine to prevent brucellosis, emphasizing the importance of proactive preventive measures.

Conclusion:
Brucellosis, though rare in certain regions, demands attention due to its potential severity and complications. By understanding the causes, symptoms, treatment options, and preventive measures outlined in this comprehensive guide, individuals can empower themselves to mitigate the risks associated with this infectious disease. Early detection, prompt treatment, and adherence to preventive practices are key to minimizing the impact of brucellosis on both individual health and public well-being.