Introduction
In the intricate landscape of reproductive health, the practice of Freezing Sperm has evolved into a valuable resource for individuals facing various life circumstances. Dr. Amin Herati, an esteemed urologist and the director of the Male Infertility and Men’s Health Clinic at Brady Urological Institute, provides valuable insights into the multifaceted reasons behind sperm banking and the intricate procedures involved.
Diverse Motivations for Freezing Sperm
- Cancer Treatment Considerations: A pivotal reason prompting individuals to freeze sperm is the prospect of undergoing cancer treatment. Dr. Herati explains that post-chemotherapy or radiation therapy, the ejaculate may have very few or no sperm left. Surgical interventions like orchiectomy, often required for testicular cancer, result in the cessation of sperm production. Hence, freezing sperm becomes a crucial measure to safeguard fertility post-treatment.
- Age-Related Fertility Preservation: The quality of sperm diminishes with age. Dr. Herati highlights that individuals, particularly those advancing in age, may opt to freeze sperm proactively to preserve their fertility as a precautionary measure.
- Medical Interventions and Occupational Hazards: Various medical procedures and conditions prompt individuals to consider sperm banking. For instance, those opting for vasectomy may want the flexibility of having children in the future. Additionally, certain medications like testosterone therapy or sickle cell therapy can impact fertility. Occupations with high risks, such as military service, may lead individuals to freeze sperm, ensuring reproductive options for themselves and their partners.
- Posthumous Sperm Retrieval: In unique and sensitive scenarios, family members may decide to collect sperm from someone who has passed away. Dr. Herati notes that sperm extraction and freezing can be carried out up to 72 hours after death, offering a unique way to preserve genetic material.

The Intricacies of Sperm Collection
The process of freezing sperm involves several crucial steps. Initially, individuals undergo infectious disease screening through a simple blood test to ensure the absence of sexually transmitted diseases. Following this, a semen sample is provided. While masturbation at a fertility clinic is the most common method, in some cases, individuals can produce a sample at home and deliver it to a lab within 24 hours.
Dr. Herati emphasizes the importance of adhering to specific guidelines during sample collection. The specimen must be placed in a lab-approved cup, maintaining proximity to body temperature. Lubricants or moisturizers are discouraged unless approved by the lab. Surgical procedures may be necessary for individuals who have undergone vasectomy, cancer treatment, or those facing infertility issues.
Analyzing and Preparing Sperm for Storage
Once the semen reaches the lab, andrologists, specialists in sperm and male fertility, conduct a meticulous analysis. They separate sperm from seminal fluid or testicular tissue and examine a small portion under a microscope. Dr. Herati explains that ensuring the presence of healthy and sufficient sperm is crucial before freezing.
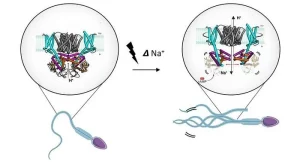
The Art of Freezing and Thawing
Sperm, prepared and separated, is placed in a special Freezing Sperm solution within small vials. These vials find their home in storage freezers containing liquid nitrogen, where sperm must remain frozen at a constant temperature of minus 196 degrees centigrade. Dr. Herati mentions that each patient’s sperm is typically split into multiple vials, stored in various tanks. This redundancy ensures the safety of sperm samples even if one freezer fails. Notably, sperm can be frozen indefinitely.
When the time comes to utilize the frozen sperm, a meticulous thawing process takes place in the lab until it reaches room temperature. Dr. Herati highlights the importance of post-thaw analysis to ensure the presence of motile, active sperm. While acknowledging that not all sperm may survive the freeze-thaw cycle, he notes that those that do may possess a fertility advantage, as studies suggest increased pregnancy likelihood when such sperm is used in in vitro fertilization (IVF).

Navigating the Financial Landscape of Sperm Freezing
The cost associated with Freezing Sperm is variable. Dr. Herati outlines that there is typically a one-time cost for sperm collection and analysis, coupled with ongoing storage costs. Storage fees can range from $100 to $500 per year. However, it’s imperative to consult with insurance providers and physicians to gain a comprehensive understanding of the financial implications.
Dispelling Myths: Can Sperm Be Frozen at Home?
Contrary to popular belief, successfully freezing sperm at home is not feasible. Dr. Herati emphasizes the necessity of laboratory settings with stringent quality controls. The average home freezer operates at about minus 18 degrees centigrade, while sperm requires storage at minus 196 degrees centigrade. However, he mentions the availability of services providing home sperm collection kits. These kits allow individuals to collect samples at home, which can then be sent to specialized labs for storage.

Addressing Fertility Concerns in the Face of a Cancer Diagnosis
For individuals grappling with a cancer diagnosis, Dr. Herati stresses the importance of initiating conversations about fertility concerns with both oncologists and fertility experts. Acknowledging that any type of cancer or treatment has the potential to impact sperm production or quality, he encourages individuals not to overlook this crucial aspect amid the concerns of cancer treatment.
Proactive Sperm Freezing for the Young and Healthy
In a proactive stance, Dr. Herati advocates for individuals between the ages of 18 and 25 to consider freezing their sperm. He contends that this age range provides an opportune window, considering the unpredictability of environmental exposures and potential health conditions. Sperm tends to be healthiest during this stage of life, making it an optimal time for fertility preservation.
In conclusion
the freezing of sperm emerges not only as a practical solution for fertility preservation in the face of medical treatments but also as a proactive measure for individuals navigating various life situations. Whether driven by age-related concerns, medical interventions, or the pursuit of family planning options, understanding the intricate process of sperm freezing empowers individuals to make informed decisions about their reproductive health, fostering a comprehensive approach to fertility management.




