Introduction:
The decision to undergo breast reconstruction after mastectomy is multifaceted. This comprehensive guide aims to provide an in-depth understanding of various options, addressing emotional, medical, and practical considerations.
Is Breast Reconstruction Right for Me?
Understanding the personal impact of living without a breast, this section delves into the emotional aspects of the decision-making process. It explores alternative choices, emphasizing the psychological benefits that reconstructive surgery can bring to individuals and their families.

Reconstructive vs. Cosmetic Surgery:
| Aspect | Reconstructive Surgery | Cosmetic Surgery |
|---|---|---|
| Purpose | Essential part of disease treatment, specifically post-mastectomy breast reconstruction | Aesthetic enhancement for personal preferences without medical necessity |
| Insurance Coverage | Generally covered by insurance as part of disease treatment | Typically not covered, considered elective and self-funded |
| Legal Classification | Recognized as a medical necessity under the law | Deemed elective, not mandated by medical necessity |
| Considerations | Focuses on restoring functionality and normalcy after surgery | Emphasizes enhancing appearance according to individual desires |
| Timing | Timing often aligned with mastectomy or post-cancer treatment | Can be scheduled at the convenience of the individual |
| Psychological Impact | Contributes to emotional well-being and sense of completeness | Aims to boost self-esteem and confidence through aesthetic changes |
| Medical Evaluation | Typically involves coordination with cancer treatment timeline | Independent of medical conditions, evaluated based on aesthetic goals |
| Insurance Approval Process | Generally straightforward due to medical necessity | May face challenges in obtaining insurance approval |
| Recovery Emphasis | Prioritizes medical and functional recovery | Focuses on cosmetic outcome and aesthetic satisfaction |
When’s the Best Time to Have Breast Reconstruction?
Timing plays a pivotal role in the breast reconstruction journey. Explore factors influencing the decision, considering ongoing cancer treatments, medical conditions, and individual preferences. Gain insights into choosing the optimal time, whether during mastectomy or post-treatment.
Different Reconstruction Options:
- Implants: Utilize silicone-gel or saline implants to restore breast shape. Involves stretching the skin with a tissue expander before implant placement.
- TRAM Flap Procedures: Use tissue from the woman’s abdomen to reconstruct the breast. Can involve pedicle or free-flap methods, each with its benefits and considerations.
- Latissimus Dorsi Flap: Takes tissue from the back to reconstruct the breast. An alternative option for those not suitable for abdominal tissue procedures.
- Aesthetic Flat Closure (AFS): Surgical repair to rearrange excess breast skin and fat after mastectomy, addressing contour deformities.
- Nipple Reconstruction: Involves creating a new nipple, either using tissue from the back or abdominal flap, or through prosthetic options. Tattooing may be used for color resemblance.

Nipple Reconstruction:
Navigate the intricacies of nipple reconstruction, examining various procedures and potential complications. Address the aesthetics and functionality of reconstructed nipples, including alternative options like prosthetic nipples.
How Long Does Breast Reconstruction Surgery Take?
Understanding the temporal aspects of breast reconstruction surgery is crucial. From the preparatory phase to the actual procedure and subsequent recovery, this section provides comprehensive insights into the timeline, aiding individuals in making informed decisions.
Recovery From Breast Reconstruction Surgery:
Explore the nuances of the recovery process, detailing postoperative discomfort, hospital stay duration, and essential post-surgery care. Emphasize the significance of self-examinations and regular medical checkups for a smooth recovery journey.
Follow-Up Care:
Highlight the necessity of ongoing medical care post-reconstruction. Encourage self-exams, regular checkups, and annual mammograms. Dispel misconceptions regarding the impact of reconstruction on cancer recurrence and ongoing treatments.

Possible Side Effects:
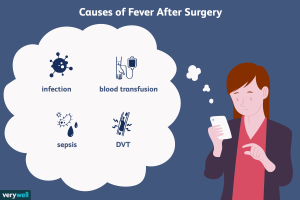
Illuminate potential side effects through a structured list:
- Infection at the surgery site
- Pain and discomfort, managed with prescribed medication
- Itching as the wound heals, with recommended ointments for relief
- Numbness or tingling due to affected nerves, lasting up to 12 months
- Fluid collection under the wound, potentially requiring drainage
- Immediate medical attention is essential for symptoms like fever, fluid leakage, color changes, increased pain, or swelling.
Conclusion:
Summarize the guide’s key takeaways, emphasizing the importance of informed decision-making and ongoing medical care in the breast reconstruction journey. Empower individuals to navigate their choices with confidence.