Introduction
Imagine fluid building up in your belly that feels milky or creamy—that’s chylous ascites. This rare form of fluid buildup happens when lymphatic fluid, rich in fats, leaks into the abdomen. Left untreated, it can cause discomfort, malnutrition, and serious health problems. But with the right approach—early diagnosis, dietary changes, and medical care—you can manage chylous ascites effectively and protect your well-being. In this comprehensive guide, we’ll demystify chylous ascites, exploring its causes, symptoms, tests, treatments, and preventive tips in clear, easy-to-understand language.
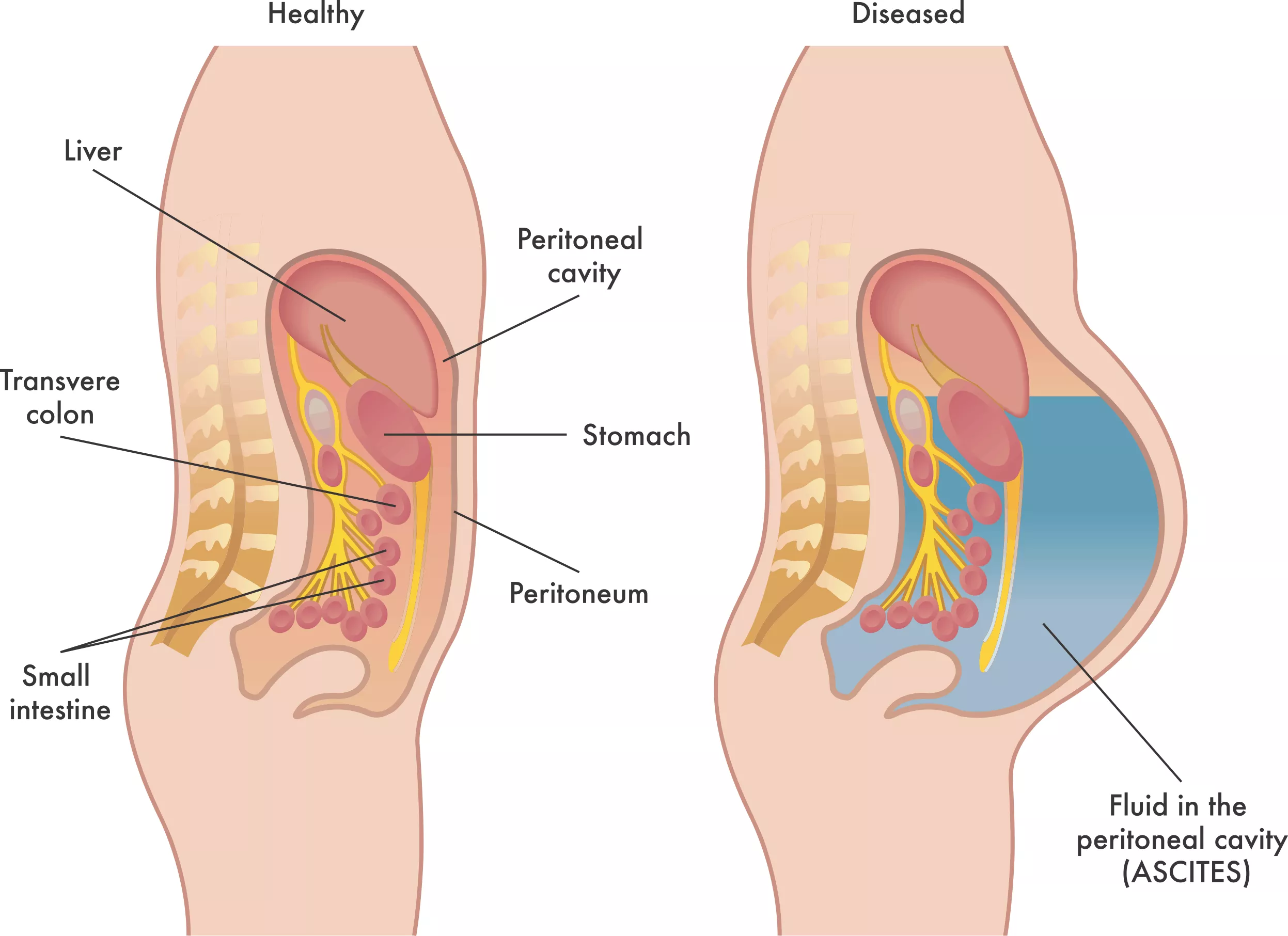
1. What Is Chylous Ascites?
Chylous ascites occurs when chyle—a milky fluid made of fats (chylomicrons), immune cells, and proteins—leaks from damaged lymphatic vessels into the peritoneal cavity (the space around abdominal organs). Unlike other types of ascites (fluid in the belly), chylous fluid is rich in triglycerides and has a distinctly cloudy look.
Key Features
- Appearance: Milky, cloudy fluid.
- Composition: High-fat (triglyceride) content, lymphocytes, proteins.
- Volume: Can range from small pockets to liters of fluid, causing visible swelling.
2. Common Causes
Several conditions can injure lymphatic channels or block lymph flow, leading to chylous ascites:
- Malignancies (Cancers):
- Lymphomas and metastatic cancers compress or invade lymph vessels.
- Trauma and Surgery:
- Abdominal surgeries, particularly around the aorta or retroperitoneum, can damage lymphatic ducts.
- Congenital Malformations:
- Rare birth defects like lymphangiectasia cause malformed lymph vessels.
- Infections:
- Tuberculosis or filariasis can obstruct lymph flow.
- Cirrhosis and Heart Failure:
- Severe liver or heart disease raises lymphatic pressure, pushing fluid into the abdomen.
Identifying the underlying cause is vital for targeted treatment.
3. Recognizing the Symptoms
Early signs may be subtle. Watch for:
- Abdominal Swelling: A visibly distended belly that worsens over days to weeks.
- Pain or Fullness: Discomfort, dull ache, or tightness.
- Digestive Issues: Nausea, poor appetite, and early satiety (feeling full quickly).
- Weight Gain: Rapid gain due to fluid, despite possible muscle or fat loss.
- Breathing Difficulty: Large fluid volumes can press on the diaphragm, causing shortness of breath.
Because chylous ascites can also lead to nutrient loss, patients may develop fatigue, muscle weakness, and vitamin deficiencies over time.
4. Diagnosis: Tests That Confirm Chyle
4.1 Physical Exam and History
A doctor will note abdominal distension, listen for fluid wave (shifting fluid when tapping one side), and ask about past surgeries, cancers, or infections.
4.2 Imaging Studies
- Ultrasound: Detects fluid pockets and guides fluid sampling.
- CT Scan: Reveals lymphatic blockages, tumors, or duct injuries.
- Lymphangiography: Specialized X-ray after injecting dye into lymph vessels to pinpoint leaks.
4.3 Fluid Analysis
A sample of ascitic fluid is key. Look for:
- Triglyceride Level: >200 mg/dL strongly suggests chylous ascites.
- Cell Count: Predominance of lymphocytes.
- Appearance: Milky or creamy color.
Additional tests check for infections (culture) and malignancy (cytology).
5. Managing Chylous Ascites
Treatment aims to reduce fluid buildup, address the cause, and maintain nutrition.
5.1 Dietary Management
- Medium-Chain Triglyceride (MCT) Diet:
- MCTs are absorbed directly into the portal vein, bypassing lymphatics.
- Foods: Coconut oil, MCT oil supplements, dairy-free formulas.
- Low-Fat Diet:
- Limits long-chain fats that enter lymph flow.
- Focus on lean proteins, fruits, vegetables, and complex carbs.
- Protein and Calorie Support:
- High-quality protein prevents muscle loss.
- Calorie-dense, low-fat snacks maintain energy.
5.2 Medications
- Diuretics (e.g., Furosemide, Spironolactone): Help remove excess fluid but may have limited effectiveness in chylous ascites alone.
- Octreotide: A somatostatin analog that reduces lymph flow and chyle production.
- Antibiotics: If infection is present or spontaneous bacterial peritonitis is suspected.
5.3 Interventional Procedures
- Therapeutic Paracentesis: Repeated drainage of fluid with a needle to relieve pain and breathing problems.
- Lymphatic Embolization: Radiologists inject glue or coils to seal leaking lymphatic vessels.
- Peritoneovenous Shunt: Surgical placement of a tube directing ascitic fluid into the venous system—used when other measures fail.
5.4 Treating the Underlying Cause
- Cancer Therapy: Chemotherapy, radiation, or surgery for lymphomas or metastases.
- Antitubercular Drugs: For tuberculosis-related obstruction.
- Surgery Correction: Repairing damaged lymphatic ducts if feasible.
6. Protecting Your Health: Preventive Tips
Even if chylous ascites arises from unavoidable conditions, you can support your body:
- Stay Hydrated: Prevents kidney strain when using diuretics.
- Monitor Abdominal Girth: Daily measurements help detect early fluid accumulation.
- Maintain Balanced Nutrition: Work with a dietitian skilled in MCT diets and micronutrient supplementation (fat-soluble vitamins A, D, E, K).
- Avoid Heavy Lifting: Prevents pressure spikes that worsen lymph leaks.
- Seek Prompt Care for Infections: Early treatment of abdominal or systemic infections reduces lymphatic damage risk.
- Regular Follow-Ups: Imaging and blood tests track progress and guide therapy adjustments.
7. Living with Chylous Ascites: Quality of Life
Coping strategies improve daily life:
- Support Groups: Connect with others facing similar challenges for emotional and practical advice.
- Physical Activity: Gentle exercise (walking, yoga) supports circulation without straining the abdomen.
- Compression Garments: Abdominal binders can ease discomfort and support posture.
- Mental Health Care: Chronic illness often brings stress or depression—counseling and relaxation techniques help maintain mental well-being.
Conclusion
Chylous ascites may sound daunting, but with swift diagnosis, nutritional management, and targeted treatments—like MCT diets, diuretics, and lymphatic interventions—you can control fluid buildup and protect your health. Identifying underlying causes, from cancers to infections, ensures precise therapies. Regular monitoring, balanced nutrition, and emotional support further enhance quality of life. By understanding the causes, recognizing symptoms early, and partnering with healthcare providers, patients can navigate chylous ascites effectively. Empowered with knowledge and proactive care, you can manage this condition and safeguard your well-being for the long term.