Can Children Really Have Depression?
Childhood depression is a distinct emotional challenge, extending beyond typical ups and downs. Recognizing the difference between occasional sadness and persistent depressive symptoms is crucial. While a child may seem sad, it’s the persistence and interference with daily life that may indicate a depressive illness. It’s essential to understand that, although serious, depression in children is treatable.
How Can I Tell if My Child Is Depressed?
Identifying depression in children involves recognizing diverse symptoms, such as crankiness, social withdrawal, changes in sleep patterns, and altered appetite. These symptoms vary, making early detection challenging. Children may exhibit different signs at different times and settings. A noticeable shift in social activities, academic performance, or appearance may indicate significant depression.

Which Children Get Depressed
Depression affects up to 3% of children and 8% of adolescents in the U.S. It’s more prevalent in boys under 10, but by age 16, girls show a higher incidence. Bipolar disorder is more common in adolescents, often accompanied by other conditions like ADHD or OCD. Risk factors include family history, substance abuse, and chaotic family environments.
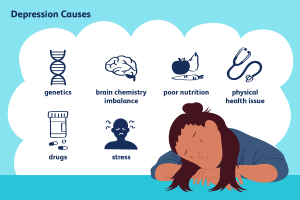
Causes Depression in Children
- Genetic Vulnerability: Children with a family history of depression are at a higher risk due to genetic factors.
- Environmental Triggers: Chaotic or conflicted family environments contribute to the development of depression in children.
- Physical Health: Poor physical health can be a contributing factor, highlighting the interconnectedness of mental and physical well-being.
- Life Events: Significant life events, such as trauma or loss, can trigger depressive symptoms in vulnerable children.
- Biochemical Disturbances: Imbalances in brain chemistry play a role, emphasizing the physiological aspects of childhood depression.

Can Depression in Children Be Prevented?
Preventing childhood depression involves identifying risk factors like family history and environmental triggers. Early intervention plays a crucial role in minimizing the risk. Acknowledging the importance of treatment and seeking professional help is vital for a child’s healthy emotional growth.
Depression Diagnosed in Children
Diagnosing depression in children requires a comprehensive approach, including medical evaluations, interviews, and mental health screenings. While there are no definitive tests, combining questionnaires with personal information aids in diagnosis. Early detection, often initiated around the 11th-year well visit, facilitates timely intervention.
Treatment Options
- Psychotherapy (Counseling):
- Utilizes Cognitive-Behavioral Therapy (CBT) and Interpersonal Therapy (IPT).
- Play Therapy is effective for younger children.
- Medication:
- Antidepressants like fluoxetine (Prozac) may be considered in severe cases.
- Caution is essential, with close monitoring for potential risks.
- Combination Therapy:
- Combining psychotherapy and medication often yields favorable outcomes.
- Family Involvement:
- Engaging families enhances support for the child’s treatment.
- Educating parents and caregivers about depression is crucial.
- School-Based Interventions:
- Collaborating with schools to create supportive environments.
- Regular communication with teachers helps monitor a child’s progress.

Long-Term Outlook
Studies indicate a trend of first-time depression occurring at younger ages. Depression may reoccur in adulthood, often coinciding with other physical illnesses. Early diagnosis, treatment, and close monitoring significantly impact long-term well-being.
Depression in Children: Warning Signs
Parents should stay vigilant for warning signs indicating potential suicidal behavior:
- Changes in eating, sleeping, and activities
- Social isolation, including from family
- Talk of suicide, hopelessness, or helplessness
- Increased undesirable behaviors
- Increased risk-taking behaviors
- Frequent accidents
- Substance abuse
- Focus on morbid and negative themes
- Talk about death and dying
- Increased crying or reduced emotional expression
- Giving away possessions
Seeking Professional Help
Encourage open communication with your child and seek professional help if needed. Address concerns and provide necessary support for your child’s mental health, even if they initially withdraw. Remember that what may seem trivial to you might feel very real to them.




