Introduction
In the intricate tapestry of global health, few threats loom as ominously as viral hemorrhagic fevers – a sinister category of illnesses known for their swift and often devastating impact. Dr. Jerry, a distinguished authority in health and wellness, guides us through the foreboding terrain of five deadly fevers, shedding light on their characteristics, origins, and the imperative for vigilance.
As we embark on this exploration, the curtain rises on a stage dominated by invisible but formidable adversaries: Ebola Virus Disease, Lassa Fever, Marburg Virus Disease, Crimean-Congo Hemorrhagic Fever, and Yellow Fever. Dr. Jerry’s expertise serves as a beacon, illuminating the intricate details of each, from their transmission dynamics to the unique challenges they pose to global health.
Beyond the shadows of these viral horrors lies a call to action – a call for awareness, preparedness, and global collaboration. This journey is not merely an unveiling of threats but an invitation to arm ourselves with knowledge, fortify our defenses, and collectively navigate the complexities of viral hemorrhagic fevers.

5 Viral Hemorrhagic Fevers
- Kyasanur Forest Disease (KFD)
- Lassa fever.
- Lujo hemorrhagic fever.
- Marburg hemorrhagic fever.
- Omsk hemorrhagic fever.
Kyasanur Forest Disease (KFD)
Transmission: Tick Bites and Animal Contact
Transmission to humans occurs through tick bites or contact with infected animals, particularly sick monkeys. Larger animals like goats may carry the virus but rarely transmit it to humans.
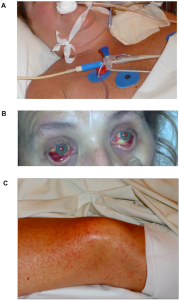
Signs and Symptoms: Waves of Illness
- Initial Wave (Days 3-8):
- Sudden onset of chills, fever, and headaches.
- Severe muscle pain, gastrointestinal symptoms, and bleeding problems may develop 3-4 days later.
- Some individuals recover after 1-2 weeks without complications.
- Biphasic Course (10-20% of cases):
- A second wave of symptoms occurs at the beginning of the third week.
- Features fever and neurological manifestations.
- Neurological symptoms include severe headaches, mental disturbances, tremors, and vision deficits.
- Outcome:
- The estimated case-fatality rate for KFD ranges from 3 to 5%.

Risk of Exposure: Geographical and Seasonal Considerations
Historically in Karnataka, KFD expanded in 2012, raising concerns about wider distribution. Outdoor enthusiasts and farmers are at risk, especially during the dry season from November to June.
Diagnosis: Early Identification is Key
Early diagnosis through molecular detection or virus isolation is crucial in the initial stages. Later stages can be identified through serologic testing using ELISA.
Treatment: Managing the Unknown
No specific treatment exists for KFD. Early hospitalization and supportive therapy, including hydration and precautions for bleeding disorders, are essential.
Prevention: Guarding Against the Unseen Threat
In endemic areas, a vaccine is crucial. Additional preventive measures include using insect repellents and wearing protective clothing in tick-endemic areas.